Contact us online
If you need help with a non-urgent medical or admin request, you can now contact us online.

Contact details and communication preferences
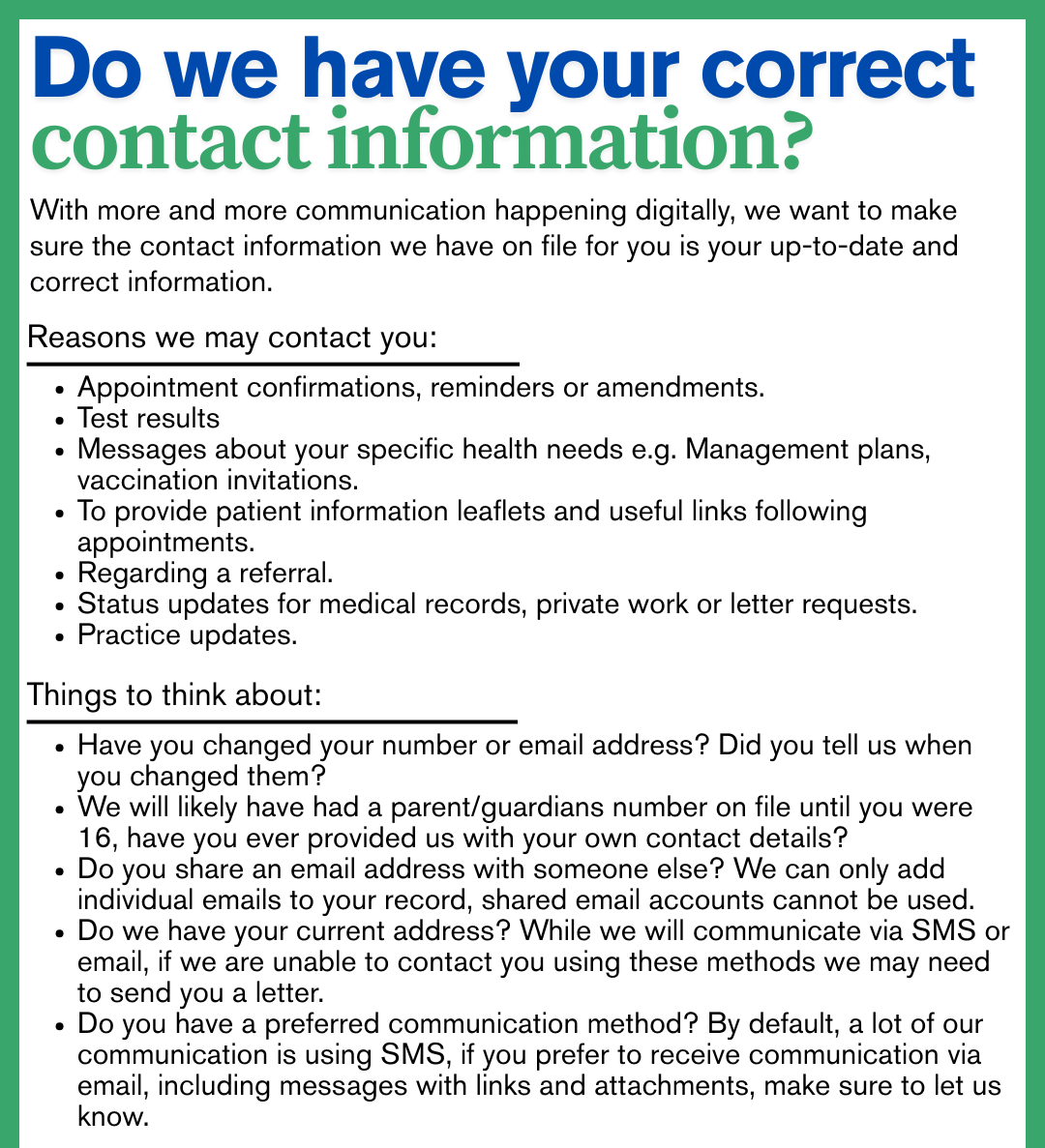
To update your details please click here: Contact details and communication preferences form
NHS App
Download the NHS App or open the NHS website up and login to access a range of NHS services online.

The practice would like to thank the various advertisers who have helped to
produce this Website. However, it must be pointed out that the accuracy of any
statements cannot be warranted, nor any products or services advertised, be
guaranteed or endorsed.